What is NTAP
The New Technology Add-On Payment (NTAP) is a reimbursement program under the Centers for Medicare & Medicaid Services (CMS) designed to provide coverage to innovative new medical services and technologies. Normally, these are covered with the standard Diagnosis-Related Group (DRG) payments. However, for very new services and technologies sometimes the costs surpass the DRG coverage, and the NTAP provides additional reimbursement to hospitals in these situations. Keep reading to find out which criteria new services and technologies need to meet to be eligible for NTAP.
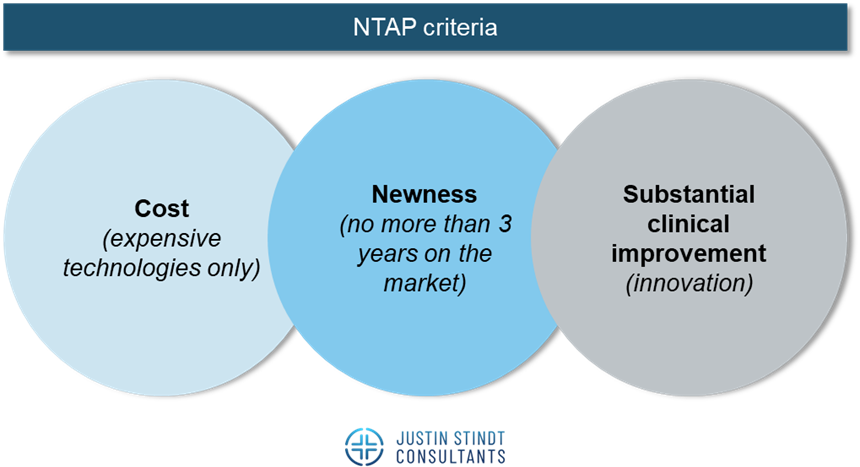
Eligibility criteria for NTAP
The substantial clinical improvement criterion
The new services and technology must provide a substantial improvement in diagnosis or treatment compared to existing alternatives. A substantial improvement is defined as one of the following:
- Treatment option for a patient (sub)population unresponsive to, or ineligible for, currently available treatments
- Ability to diagnose a currently undetectable medical condition, or ability to diagnose earlier than with currently available methods and there must also be evidence that the use of the new technology affects the management of the patient
- Significant improvement of clinical outcomes compared to alternatives as demonstrated by one or more of the following outcomes:
- A reduction in at least one clinically significant adverse event, including a reduction in mortality or a clinically significant complication
- A decreased rate of at least one subsequent diagnostic or therapeutic intervention
- A decreased number of future hospitalizations or physician visits
- A more rapid beneficial resolution of the disease process treatment including, but not limited to, a reduced length of stay or recovery time
- An improvement in one or more activities of daily living
- An improved quality of life
- A demonstrated greater medication adherence or compliance
To evaluate the new service or technology, evidence from published and unpublished sources from the US or elsewhere will be used. These sources may include clinical trials, peer-reviewed journal articles, study results, meta-analysis, consensus statements, white papers, patient surveys, case studies, reports, systematic literature reviews, letters from major healthcare associations, editorials and public comments (not exhaustive).
Newness criterion
The newness criterion ensures that NTAP is reserved for truly innovative and new services and technologies. To quality for NTAP, the technology must be considered “new” by CMS, which means no more than 2-3 years passing from the date on which an inpatient hospital code is issued. After this period ends, the code is recalibrated to more accurately reflect the cost of the service or technology. As a result, the service or technology is no longer considered “new” and the manufacturer must seek reimbursement through standard payment mechanisms.
In addition to the time consideration, a technology is not considered new if: (1) it uses the same or similar mechanism of action as an existing technology, (2) it has been assigned to an existing MS-DRG, and (3) it treats the same or similar type of disease and patient population as an existing technology.
Cost criterion
The NTAP is designated primarily for new high-cost services and technologies and there is a criterion to determine which new services and technologies qualify for the additional payment. The cost criterion evaluates whether the cost of the new technology or service exceeds the predefined 75% cost-to-charge thresholds established with the release of the most recent annual IPPS final rule. This threshold is calculated as a percentage of the Medicare Severity-Adjusted Diagnosis-Related Group (MS-DRG) payment amount. The cost of the technology is calculated as the list price of the technology minus any discounts or rebates that hospitals typically receive. CMS uses this adjusted cost to determine whether the threshold is met.
Alternative pathways for NTAP
Certain new medical services and technologies may be eligible to apply for NTAP under an alternative pathway. For example, technologies that receive the FDA’s Breakthrough Device Designation are eligible for NTAP based on their innovative nature and potential to address unmet clinical needs. CMS acknowledges the rigor of the FDA’s breakthrough designation process and waives the requirement for the applicant to independently demonstrate substantial clinical improvement. Further, technologies designated as Qualified Infectious Disease Products (QIDP) are automatically considered for NTAP without the need to demonstrate substantial clinical improvement because these products often address significant public health challenges, such as antibiotic resistance.
Even though these products do not need to demonstrate the substantial clinical improvement criterion, they still need to satisfy the cost criterion and the newness criterion.
How can companies apply for NTAP
Applicants for NTAP need to receive the FDA marketing authorization by May 1st of the year prior to the beginning of the fiscal year for which the application is being considered (not necessary for the QIDP/LPAD pathways). The NTAP application must include comprehensive documentation to support the technology’s eligibility. For example, the dossier must include a description of the technology, mechanism of action, information on the FDA approval, and cost analysis (not exhaustive).
For a comprehensive overview of all mandatory and supporting documentation, please reach out to us.
Applications are submitted to CMS during the annual NTAP application window which is typically due by early October for the following fiscal year. Applications for FY 2026 have already passed, stressing the importance of planning your submission well in advance. Applications must be submitted electronically through the designated CMS portal. CMS issues its final decision on NTAP applications in the IPPS final rule, typically released in August.
JSC Expertise
Justin Stindt Consultants is a specialized market access consulting firm offering bespoke market access services. Our team of experts has extensive experience in US Market Access, ensuring that our clients are well-prepared for seamless application submissions. Our agency has been the preferred service provider for many medtech and pharma companies seeking assistance with crafting the US Market Access strategy.
Stay Updated
We are closely tracking all US news and changes relevant to our medtech clients. For more detailed insights and updates, visit our blog regularly.
Why Choose Us?
- Proven Expertise: With years of experience in global pricing and reimbursement, our team offers unparalleled expertise and strategic insights.
- Tailored Solutions: We understand that each client and market is unique, and we provide customized solutions that address specific needs and challenges.
- Comprehensive Support: From initial strategic advice to implementation and beyond, we offer end-to-end support to ensure your success.
- MCO and Regulatory Mastery: Our deep understanding of regulations, requirements and processes, including extensive experience with the FDA and American payers, positions us to effectively support Market Access and coverage for your products.
Partner with Justin Stindt Consultants to leverage our expertise and achieve your market access goals with confidence.